Insulin resistance and diabetes are well-known and well-documented conditions. Diabetes affects 463 million people worldwide! But what really is insulin resistance and how does it play a role in modern diseases like metabolic syndrome and type 2 diabetes?
Insulin and The Pancreas
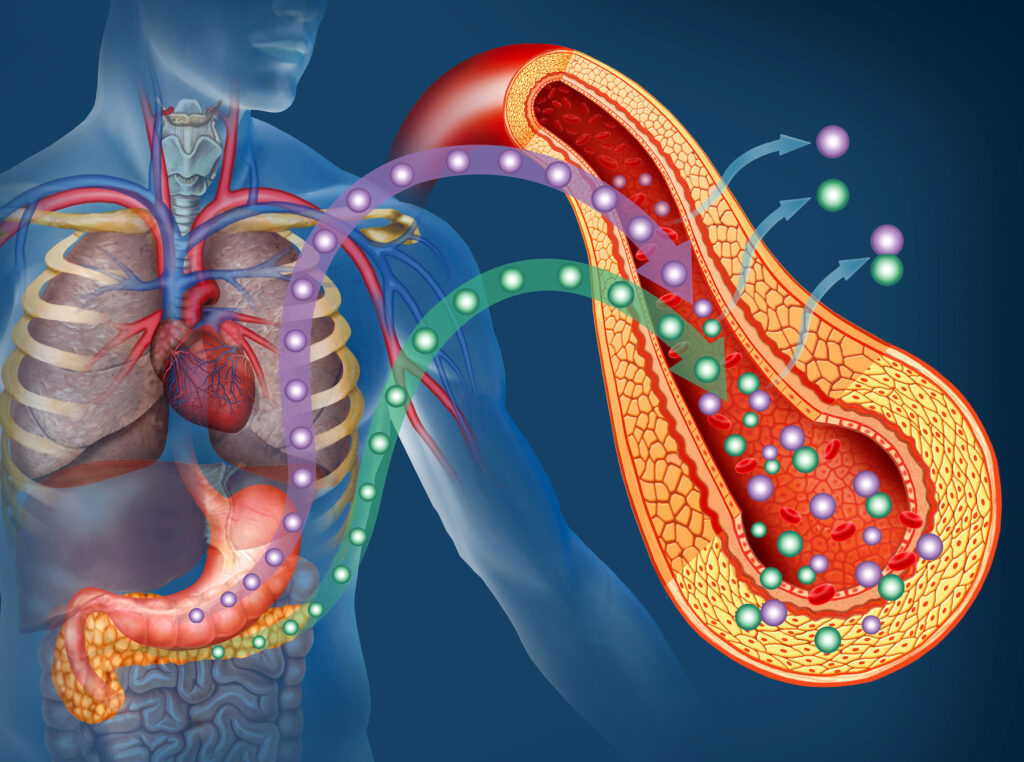
The pancreas is an organ that sits in your upper abdomen and produces an important hormone that regulates blood glucose levels – insulin. Insulin allows glucose to enter cells to provide the energy they need.
Normally, insulin is tightly regulated so the body stays in metabolic balance. When you eat a meal, the food breaks down into a usable form of energy called glucose. Glucose enters the bloodstream, signaling the pancreas to release insulin. Then insulin helps glucose get into the body’s cells so it can be used for energy right away or stored for later use. Once glucose enters the cells, levels of glucose drop in the bloodstream, signaling to the pancreas to stop producing insulin. This is how the feedback loop normally works. However, this process can become out of balance with a diet high in sugars, alcohol, and high processed packaged foods.
What is Insulin Resistance?
Put simply, insulin resistance is when the body responds improperly to insulin. This causes muscle, fat, and liver tissues to not respond adequately to normal insulin levels – leading to higher baseline blood sugar levels, especially after meals high in carbohydrates. To compensate, higher amounts of insulin are needed to maintain metabolic balance. This puts more burden on the pancreas to increase insulin output. As long as the pancreas can continue to make enough insulin, it can overcome this and keep blood sugar levels in a healthy range.
However, if the cells become resistant to insulin, elevated blood glucose levels occur. This can be either temporary or chronic. Temporary insulin resistance often occurs from the use of certain medications, like oral steroids for example, or a meal very high sugars or refined grains. But if chronic, insulin resistance may lead to prediabetes and type 2 diabetes over time.
Testing for Insulin Resistance
Fasting Blood Glucose
A very common and simple blood test to look at levels of glucose in the blood after an overnight fast can be helpful. A normal blood glucose is less than 100mg/dl. More optimal is less than 90. If the fasting blood glucose is higher than 100, it may indicate insulin resistance. However, there are several other factors that can influence the morning fasting blood glucose, such as poor sleep, stress, and certain key nutrient deficiencies to name a few.
Fasting Insulin Levels
Checking a fasting insulin level is another blood test that can be helpful in assessing metabolic balance. Normal fasting insulin levels are on most standard labs is less than 25, however a healthier insulin level is below, and some metabolic experts say to aim for a level of 7 or less. If insulin levels start to rise, it means the pancreas is putting out more insulin in an attempt to lower the higher glucose levels in the blood.
Hemoglobin A1c (HbA1c)
A blood test called HbA1c, or glycated hemoglobin A1c, helps to diagnose prediabetes or diabetes. It shows the average blood sugar level over the last three months. Since it looks at levels over time it is of course of a longer period time, it is not reflective of short-term changes like fasting glucose can be.
- Normal = HbA1c < 5.7%
- Prediabetes = HbA1c between 5.7 and 6.3
- Type 2 diabetes = HbA1c > 6.3
- Optimal= HbA1c 5.4% or less
Oral Glucose Tolerance Testing (OGTT)
Oral glucose tolerance tests are used to measure how well the body can process a larger amount of sugar. If the blood sugar measured in the test is above a certain level, this could be a sign that sugar is not being absorbed enough by the body’s cells. After that you drink a large glass of concentrated sugar solution, blood is drawn again after two hours and three hours and the blood glucose level are measured. If you have prediabetes, you’re at risk of eventually developing type 2 diabetes. You’re also at risk of developing heart disease, even if you don’t develop diabetes.
- A normal blood glucose level is lower than 140 mg/dL (7.8 mmol/L).
- A blood glucose level between 140 and 199 mg/dL (7.8 and 11 mmol/L) is considered impaired glucose tolerance, or prediabetes.
- A blood glucose level of 200 mg/dL (11.1 mmol/L) or higher may indicate diabetes.
Prediabetes and Type 2 Diabetes
Prediabetes
In prediabetes, cells don’t respond normally to insulin, so the pancreas makes more insulin to trigger a cellular response. When the pancreas can’t keep up, blood glucose levels rise. In the prediabetic stage, blood glucose levels are higher than normal, but not high enough to be diagnosed with type 2 diabetes. Oftentimes, there are no clear symptoms of prediabetes and it’s not detected until the person develops type 2 diabetes.
Risk factors for prediabetes include:
- Being overweight, especially with excess body fat around the stomach (visceral fat)
- Lack of physical activity
- Family history of type 2 diabetes
- Standard American diet of processed foods with low nutrient value
Type 2 Diabetes
Type 2 diabetes occurs with chronic high blood glucose levels, diagnosed with a HgA1c level of over 6.3. Type 2 diabetes often occurs in adulthood and is associated with poor lifestyle choices, especially a poor diet and lack of enough exercise.
Symptoms of type 2 diabetes include:
- Increased thirst and/or urination
- Fatigue
- Blurred vision
- Increased hunger
- Unexplained weight loss
Type 1 Diabetes
Type 1 diabetes is a bit different. It’s an autoimmune disease that occurs when the immune system attacks and destroys insulin producing cells in the pancreas. Because the insulin-producing cells can’t function properly, injectable insulin is required to maintain healthy blood glucose levels. GAD65 antibodies are present in type 1 diabetes, so a GAD65 test is a specific blood test that can be done to indicate the presence of type 1 diabetes.
Common Oral Medications for Insulin Resistance and Diabetes
Traditionally, oral medications are used for insulin resistance and diabetes treatment. These medications can either stimulate secretion of insulin in the pancreas or increase insulin sensitivity.
Common medications include:
- Metformin. One of the most common prediabetes/type-2 diabetes medications, Metformin has been used for over 60 years because it’s highly effective at reducing blood glucose levels.
- Sulfonylureas medications. This group of diabetes medications decrease blood glucose by stimulating the beta cells of the pancreas to release insulin. These can also increase the risk for hypoglycemic events (low blood glucose), overwork your pancreas, and encourage insulin resistance.
- Glitazones. These medications reduce circulating fat cells and improve the body’s sensitivity to insulin.
- Glinides, or meglitinides, release more insulin into the blood so glucose levels decrease.
- Gliptins (DPP-4 inhibitors), a newer form of diabetes medication, are often prescribed when the patient hasn’t responded well to other medications like metformin.
- Gliflozins, also known as SGLT-2 inhibitors, lower HgA1c and blood glucose levels without causing hypoglycemia. These are also used in the treatment of heart failure.
- GLP-1 agonists help regulate blood glucose and HgA1c levels. The hormone GLP-1 is a critical part of the pathway for insulin secretion by the pancreas. They are also FDA approved for weight loss.
- Insulin is normally secreted by the pancreas but can also be taken as a medication to help the body use glucose effectively and avoid high blood glucose levels. When taken as a medication, insulin often causes weight gain. However, in the case of Type 1 Diabetes taking insulin is necessary and lifesaving as the pancreas is no longer secreting any insulin.
Functional Medicine Treatment for Insulin Resistance
Diet Change
A diet high in processed carbohydrates, fast foods, and sugars cause blood sugar levels to spike. This puts stress on the pancreas to produce lots of insulin and can lead to insulin resistance. Decreasing carbohydrates, sugar, and processed foods can help significantly!
Other diet changes that can help include:
- Lowering alcohol intake.
- Decreasing carbohydrates and sugars.
- Increasing fiber-rich foods like fresh vegetables and fruits. Aim for at least 35 grams of fiber daily.
- Increasing lean protein.
- Intermittent fasting.
Exercise
Exercise is helpful for improving insulin resistance, particularly weightlifting and high-intensity interval workouts (HIIT). Studies have found that increasing muscle mass can reduce lipid accumulation in muscle cells and improve insulin resistance. 150-300 minutes per week of moderate intensity exercise is ideal.
Correcting Key Nutrient Deficiencies in Insulin Resistance
Researchers believe that because of its anti-inflammatory properties, vitamin D3 may protect against insulin resistance.
A deficiency of zinc can decrease the body’s response to insulin. Zinc supplementation helps maintain glucose balance and metabolic homeostasis.
Magnesium helps regulate blood glucose levels. When levels of magnesium are low, insulin resistance is more common.
Supplements For Insulin Resistance
Key glucose and insulin balancing supplements include:
- Chromium helps reduce insulin resistance and positively impact type 2 diabetes. Most studies recommend 200mg of chromium 1-3 times daily.
- Berberine improves cellular response to insulin by inhibiting the storage of fat. When taken over a three-month period, patients had reduced waist circumference and BMI.
- Alpha lipoic acid is shown to improve insulin resistance by playing a role in the insulin signaling pathway.
- Cinnamon can decrease fasting blood glucose levels and improve insulin sensitivity.
- Gymnema supports glucose metabolism and positively impacts metabolic syndrome.
- Ginseng, an herb with antidiabetic effects, improves glucose tolerance and insulin resistance.
Arizona Wellness and Our Functional Medicine Approach to Insulin Resistance
Insulin resistance can happen to anyone if they aren’t careful with their diet and lifestyle. Whether it’s temporary or chronic, insulin resistance is a serious condition that should be treated with care.
If you’ve been struggling with insulin resistance, have tried oral medications in the past, or want to lower your HbA1c level naturally, functional medicine can help. Our team of functional medicine providers at Arizona Wellness Medicine work with patients everyday who have insulin resistance. Learn more about how we can create a personalized plan for your insulin resistance here.
Resources:
- Pancreas Hormones
- Metformin and Its Benefits for Various Diseases
- DPP-4 Inhibitors (Gliptins)
- Gliflozins in the Management of Cardiovascular Disease
- Insulin Resistance: From Mechanisms to Therapeutic Strategies
- Prediabetes
- Type 2 Diabetes
- GAD65 autoantibodies and its role as biomarker of Type 1 diabetes and Latent Autoimmune Diabetes in Adults (LADA)
- Low Vitamin D May Contribute to Insulin Resistance
- Zinc and Insulin Sensitivity
- Molecular Mechanisms of Chromium in Alleviating Insulin Resistance