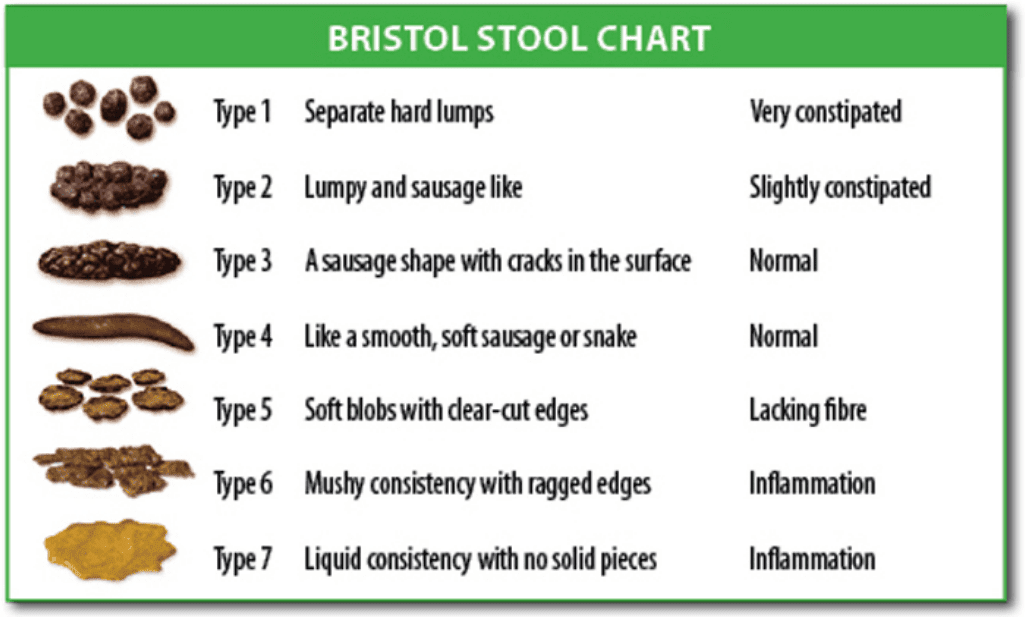
OK, so I know poop is not at the top of the conversation list, however, it is an important part of health, I promise! Eighty percent of your immune system is located in your gut, making what is inside your intestines critical. Your stool can reveal a lot about your health. First let’s review what normal stool should look like. Since stool is 75% water, it is no surprise that it should be smooth, soft, and semi-formed. It should also come out in one long piece, and be medium to light brown in color, with a natural smell. For a visual, see the Bristol Stool Chart below. It is optimal to have 1-3 bowel movements per day. Stool is one of your body’s main ways to detoxify, so if you aren’t going at least once every day, you may not be eliminating toxins in the most efficient manner.
 If you are not having a minimum daily bowel movement, you likely have a form of constipation, and should first evaluate your water intake. The goal is at least half your body weight in ounces, more it you are active and/or if it is hot out. Next, evaluate your plant fiber intake, and make sure you are getting 10 or more servings of plant foods per day, mostly vegetables. Exercise and movement also help with achieving normal bowel movements, as do deep breathing and relaxation exercises, because they help balance the nervous system, particularly the parasympathetic nervous system, which helps you rest and digest. There is a huge branch of this nervous system inside the gut, called the enteric nervous system, which controls many aspects, including motility. Motility refers to how fast your intestines contract and relax to move food and stool through the system through a sequence of movements called peristalsis, and is an important part of gut health. Medications and supplements can affect motility, and cause constipation as a side effect. Pain medications such as opioids commonly cause constipation, as can supplements containing iron and calcium.
If you are not having a minimum daily bowel movement, you likely have a form of constipation, and should first evaluate your water intake. The goal is at least half your body weight in ounces, more it you are active and/or if it is hot out. Next, evaluate your plant fiber intake, and make sure you are getting 10 or more servings of plant foods per day, mostly vegetables. Exercise and movement also help with achieving normal bowel movements, as do deep breathing and relaxation exercises, because they help balance the nervous system, particularly the parasympathetic nervous system, which helps you rest and digest. There is a huge branch of this nervous system inside the gut, called the enteric nervous system, which controls many aspects, including motility. Motility refers to how fast your intestines contract and relax to move food and stool through the system through a sequence of movements called peristalsis, and is an important part of gut health. Medications and supplements can affect motility, and cause constipation as a side effect. Pain medications such as opioids commonly cause constipation, as can supplements containing iron and calcium.
Other medical conditions such as hypothyroidism, food sensitivities, or nutrient deficiencies may also be contributing to constipation. An easily overlooked factor is related to optimal position during a bowel movement, especially if constipation is an issue. Devices such as the Squatty Potty put you in the correct position for proper stool elimination, and can be a helpful part of your treatment regimen.
On the flip side, if you are having more than 3 loose bowel movements per day, it is also a sign that gut health is not optimal. Diarrhea can be a sign of a serious condition like an inflammatory bowel disease, such as crohn’s disease, ulcerative colitis or celiac disease for example. Irritable bowel syndrome, gut infections, or hyperthyroidism are also potential causes, as well as other conditions such as cystic fibrosis, and gallbladder disease. It can also be induced by food sensitivities, anxiety, extreme exercise, adding too much fiber to the diet too quickly, and of course by medications and supplements. For example, magnesium is a common nutrient deficiency, and often requires supplementation over long periods of time to fully replenish nutrient stores inside the cells. I often have my patients use loose stools as a guide to help determine proper magnesium dosing. However, too much magnesium, especially in the form of magnesium citrate, can also cause diarrhea, and is sometimes used as a treatment for constipation. Some common medications that cause diarrhea are antibiotics and drugs to treat cancers. If you are taking these medications you can help mitigate diarrhea by taking a good quality multi-strain probiotic containing lactobacillus and bifidobacterium species. If you have been on multiple courses of antibiotics, or have recently taken or are taking clindamycin and are experiencing diarrhea, I advise asking your healthcare provider for a stool study to look for clostridium difficile (c.diff), which is a bacteria that can be difficult to treat when overgrown in the gut due to antibiotics killing off healthy gut bacteria, allowing this one to flourish. If you have known c.diff, or have to take clindamycin for an infection, you will want to add saccharomyces boulardii (sac b) to your probiotic to make it more effective in preventing and treating diarrhea.
How do we evaluate and treat constipation and diarrhea in functional medicine? Evaluation of a bowel disturbance often requires blood work and stool studies to start, and may require imaging such as a CT scan or MRI, or an endoscopy and referral to a gastroenterologist depending on the frequency and severity of symptoms. In my functional medicine practice it is fairly common to see patients that have already had a full traditional work up that is negative, yet are still having unresolved gut issues. This is where we will dig in (there is actually a pneumonic we use called DIGIN in functional medicine) to find the root causes of your signs and symptoms. Using the functional medicine timeline and matrix to take a complete history and organize the data, as well as a comprehensive physical exam are the first steps. Next, you will get a personalized, science based healthcare plan, including any advanced laboratory investigation needed. Your functional medicine plan is also certain to contain specific lifestyle recommendations on nutrition (likely an elimination diet), sleep, exercise, and stress management, as well as any necessary medications or nutritional supplements for optimal gut function. These are the initial steps to getting you well on your way to health, and will be followed by further specific testing, evaluation, and adjustments to your individual plan as needed. Remember, in functional medicine the goal is to optimize all aspects of health and wellness, to help you feel better in the short term, AND to prevent chronic diseases and illness in the long term.