Menopause is a normal life event for women, a time when childbearing years come to an end and a new life stage begins. But for some, symptoms can be severe and take a toll on their quality of life – hot flashes, mood changes, poor sleep quality like waking many times during the night, night sweats, and joint pain can make normal life difficult. This is where hormone replacement steps in – it can help manage unwanted symptoms and supports hormone regulation in the body.
But what really is hormone replacement therapy? Is it safe? Let’s look at what bioidentical hormone replacement therapy actually is and what the research says.
What is Bioidentical Hormone Replacement Therapy?
Bioidentical hormones are artificial hormones created from plants. They are very similar to those created in the body, helping to balance out abnormalities. Bioidentical hormones can include estrogen, progesterone, and testosterone and are used as a replacement therapy during or around menopause when unbalanced hormone levels cause a variety of frustrating symptoms like hot flashes, mood changes, and poor sleep for example.
Despite the media portraying misinformation about hormone replacement in the last couple of decades causing some to be wary, it’s generally safe. Research even reports that it plays a significant role in improving quality of life for those who take it. If that’s not enough, it also helps prevent coronary heart disease, improves brain health, reduces overall mortality, and minimizes the risk of osteoporosis and fractures.
Who Would Benefit the Most from Hormone Replacement Therapy?
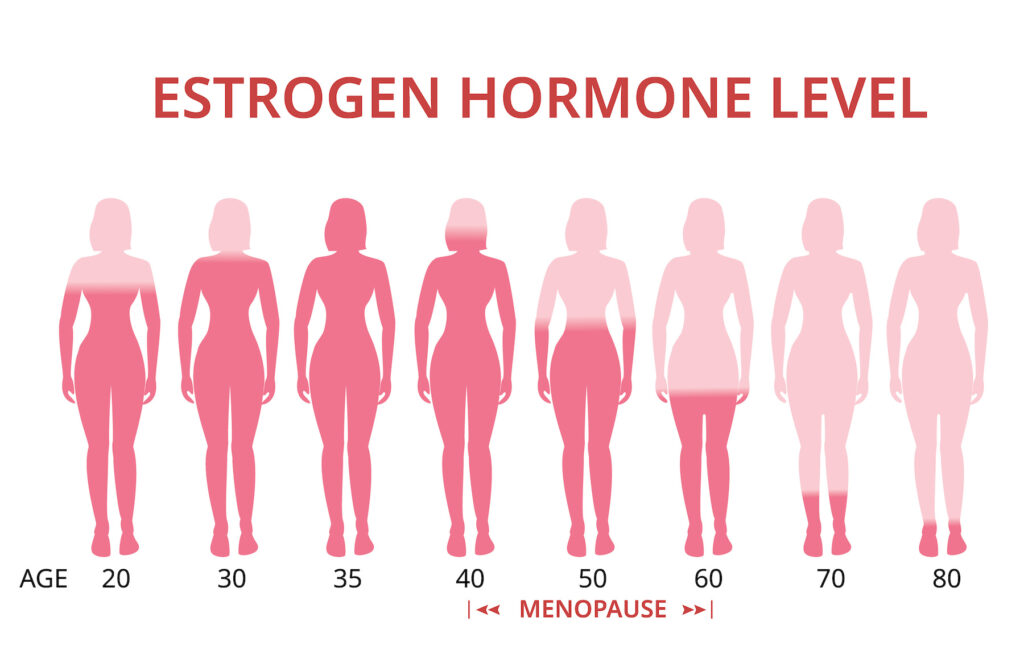
Bioidentical hormone replacement therapy is best for women in their first 10 years of menopause, who are under the age of 60. This is because of the vast hormone changes occurring in menopause.
During menopause, a significant drop in estrogen and progesterone occurs. It’s the drop in estrogen levels that causes many of the difficult symptoms like hot flashes and night sweats. So, when taken around the time of menopause, bioidentical hormone therapy can help balance out the changes in hormones, leading to less frustrating symptoms and more relief.
Types of Bioidentical Hormone Replacement Therapy Used in Menopause
Estrogen replacement is the most commonly used hormone therapy in the US. The term estrogen is a general term, as there are different forms. Estrone, estradiol, and estriol are the 3 types. When doing hormone replacement therapy estradiol or a combination of estradiol and estriol are commonly used. Estrogen is usually prescribed transdermally via a topical cream or a patch.
Progesterone is the other commonly used hormone replacement for menopausal women. It can be either oral micronized progesterone or synthetic progestin. Micronized progesterone is identical both chemically and structurally to the progesterone produced in the body, so is preferred for bioidentical hormone replacement, as the synthetic progestins tend to come with increased risk of side effects.
What Are the Risks of Bioidentical Hormone Replacement Therapy?
Older studies looking at synthetic estrogens and progestins found increased risks of certain cancers and blood clots. But the good news is, recent studies completed with bioidentical hormones don’t show these risks. In fact, one study completed over an 18 year period by the Women’s Health Initiative, noted that women taking bioidentical hormone replacement therapy did not have a higher risk of cardiovascular disease, cancer, or all-cause mortality risk than women not taking it.
While many of the risks previously associated with synthetic hormone replacement have not been shown to be relevant to bioidentical hormone therapy, your provider will still ask about any history of stroke, cardiovascular disease, cancer, or blood clotting disorder before prescribing to make sure your risk of these occurring isn’t too high.
What Are the Benefits of Bioidentical Hormone Replacement Therapy?
There are many benefits of bioidentical hormones replacement therapy, including:
- Reduced cardiovascular risks like heart attack, stroke, and blood clots.
- Improved bone density with reduced risk of osteopenia and osteoporosis
- Improved sleep quality
- Improved mood
- Improved cognition and brain health – One study found that women taking hormone therapy had a decreased risk of Alzheimer’s disease when compared to women not taking hormone therapy.
- Reduction in all-cause mortality for women in their first 10 years of menopause, who are under the age of 60.
That’s a pretty amazing list!
Bone health is one area that’s especially promising, as older women tend to be at a higher risk for falls and fractures. So much so that menopausal women are the majority of those with osteoporosis! But this risk decreases for those taking bioidentical hormone therapy. This is because estrogen helps slow the breakdown of bones by inducing cell death or apoptosis of osteoclasts, which are cells that degrade bone. This protective mechanism works to prevent further bone loss. Studies have found that hormone replacement significantly decreases risk of hip and vertebral fractures, a great benefit for this age group. This is especially important given the increased risk for poor longevity and lifestyle outcomes for patients who have undergone surgery for hip fractures.
Mood changes can also be common for women in the perimenopausal stage. Progesterone can help with this, as it offers an anti-anxiety effect because it promotes GABA, which has a calming effect. There is also promising evidence that hormone therapy may have potential antidepressant effects when given to menopausal women with depression!
How Do You Take Bioidentical Hormones?
Bioidentical hormone replacement can be taken in several different ways – orally or transdermally. But not all hormones should be taken both ways because of certain risks.
Oral estrogen, for example, is not recommended because of an increased risk of venous thromboembolism, or blood clots in the legs, and stroke. This is especially true for people with a BMI over 30. For this reason, transdermal estrogens are recommended – usually as estradiol or a combo of estradiol and estriol. Studies have shown no association between increased venous thromboembolism and transdermal estrogens.
Synthetic progestins are also not recommended orally because of an increased risk of venous thromboembolism and breast cancer risk. But, oral micronized progesterone, which is the recommended form of progesterone, can be taken orally and is recommended because it doesn’t have any of these increased risks of venous thromboembolism, breast cancer, or cardiovascular risk. Plus, it doesn’t impact blood pressure. Oral micronized progesterone even provides endometrial protection for those taking estrogen with a uterus – or in other terms, those who haven’t had a hysterectomy.
How Functional Medicine Can Help You Balance Your Hormones
If you’re struggling with menopause symptoms like hot flashes, night sweats, mood changes, or loss of energy, maybe it’s time to consider how bioidentical hormone replacement could help. You’ll ideally want to do blood work and some advanced hormone metabolism testing, such as the DUTCH (dried urine testing for comprehensive hormones) test.
Functional medicine can provide a window into what’s going on in the body by taking a holistic approach. It looks at the whole picture to get a complete picture of your health history, your current symptoms, your diet, and more. That’s why at Arizona Wellness Medicine, we treat health as multi-functional, so we can get to the bottom of your symptoms to find lasting relief. Learn how our functional medicine providers at Arizona Wellness Medicine can help you here.
Resources:
- Effectiveness of transdermal oestradiol and natural micronised progesterone for menopausal symptoms
- Risks, Benefits, and Treatment Modalities of Menopausal Hormone Therapy: Current Concepts
- Cognition, Mood and Sleep in Menopausal Transition: The Role of Menopause Hormone Therapy
- Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease: It’s About Time and Timing