It’s the end of a long workday, and you’re ready to get to bed. But the pain and stiffness in your knee make it difficult to get comfy and actually rest.
Ouch!
You reach for an ice pack and some over-the-counter ibuprofen. Finally, after 30 minutes, you drift off the sleep.
What could possibly be causing the pain?
Your pain may be caused by arthritis. Arthritis is when your joints become inflamed leading to pain and stiffness. There are different types of arthritis including autoimmune arthritis like rheumatoid arthritis, juvenile arthritis, post-traumatic arthritis, and osteoarthritis for example.
The most common type of arthritis is osteoarthritis. It affects over 32.5 million adults in the United States. So there’s a good chance your pesky knee pain could be caused by osteoarthritis. In that case…
- What exactly is osteoarthritis?
- How is it different from other types of arthritis?
- What causes osteoarthritis?
- Who’s at risk for this common disease?
- What are natural ways that you can improve your symptoms if you’re suffering from osteoarthritis?
Let’s wave those painful nights goodbye and explore these questions!
What Is Osteoarthritis?
To start, let’s break up the word “osteoarthritis” into two parts:
- “Osteo” means relating to the bone
- “Arthritis” means tenderness and swelling of one or more joints
So, osteoarthritis is a type of arthritis that involves the actual bones in your joints. Its common symptoms include:
- Joint pain and stiffness that gets worse with intense activity
- Deformity of joints or reduced joint function
Osteoarthritis can be diagnosed through a medical exam by your doctor. An x-ray can be done to confirm it. What will the x-ray show you? Keep reading to find out.
What Causes Osteoarthritis?
Medical professionals commonly call osteoarthritis the “wear and tear arthritis.” Just like a 20-year-old car won’t function like it did when you drove it off the lot, your body ages over time.
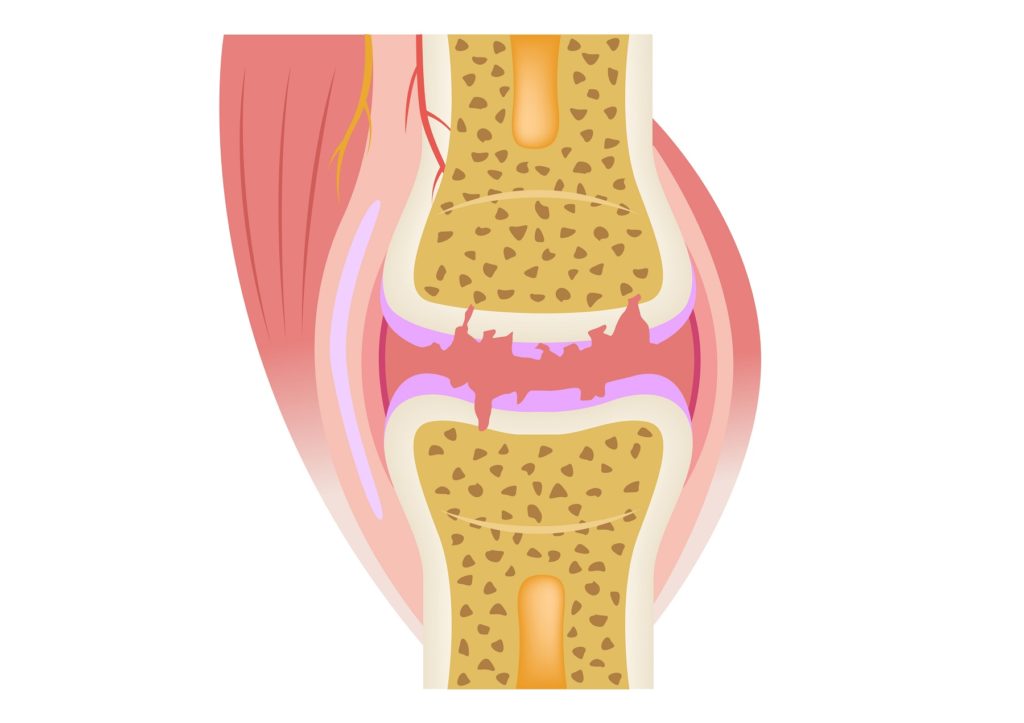
One body tissue that ages is your cartilage. Your cartilage acts as a cushion between the bones in your joints. In osteoarthritis, the cartilage in your joints gets worn down to the point where the bones are directly touching each other. There’s no more cushion to protect your bones as you move your joints, so the bone tissue gets damaged and inflamed, which causes the pain.
Osteoarthritis can affect your joints such as your ankles, knees, hips, spine, wrists, and the joints in your fingers.
Let’s take the joint in your knee for example. A healthy knee x-ray will show space between the two bones connecting your knee. Just like your middle school teacher telling you to create space between you and your date, space is a good thing. This space means there’s still cartilage that’s protecting your bones from touching each other.
In a knee with osteoarthritis, there’s no space. Bone-on-bone contact causes the pain you’re experiencing. You may also see small pieces of bone called osteophytes that are coming out of the joint.
While age is the number one factor for people getting osteoarthritis, there are some people who are more at risk than others for getting the disease.
Who Is at Risk for Osteoarthritis?
Risk factors for osteoarthritis include:
- Age: The more you age, the more likely your cartilage is deteriorating because you’re constantly using your joints for everyday activities.
- Obesity: More weight and force are being placed on your body’s joints, which can lead to faster “wear and tear.”
- Occupation: If you have a very active job that involves heavy lifting, your joints may be at risk of overuse. If you put repetitive stress on your joints, you can easily damage them and you’re at risk of osteoarthritis. These jobs may include workers in construction, firefighting, agriculture, fisheries, forestry, and mining.
- Gender: Women are more likely to be diagnosed with osteoarthritis than men. This may have to do with changing hormone levels and bone health.
- Genetics: If osteoarthritis runs in your family, you may be more likely to develop it.
If you have osteoarthritis or you’re at risk of developing it, there are natural ways to improve and treat your symptoms.
Treatment for Osteoarthritis
Processed and packaged foods tend to be high in artificial ingredients, refined carbohydrates, and trans fats. While they may be convenient to eat, your body doesn’t thrive off these foods. In fact, eating highly processed foods can increase inflammation.
Sugars can also increase your inflammation. This doesn’t help with osteoarthritis because these foods will increase the inflammation in your joints which increases pain. Plus, sugary processed foods contain no nutritional value.
To treat and prevent osteoarthritis, eat an anti-inflammatory diet. These include foods and spices such as:
- Ginger
- Turmeric
- Green tea
- Avocados
- Beets
- Blueberries
- Walnuts
- Salmon
- And even some 70% or higher Dark chocolate
Adding these foods to your diet along with refraining from processed foods will go a long way in helping your body heal from and prevent osteoarthritis.
- Supplements
I recommend a number of supplements to my patients for osteoarthritis. Some of these include:
- Curcumin (found in turmeric): Curcumin produces analgesic (relieves pain) and anti-inflammatory effects. Using curcumin is a great alternative to analgesic drugs because these drugs can have adverse effects on our body’s systems like our hepatic system.
- Boswellia: Boswellia is also known as Indian frankincense. It’s been used for centuries in Asian and African countries to treat chronic inflammation. Studies have shown that Boswellia used in combination with curcumin reduces pain in patients with osteoarthritis.
- Omega-3 Fatty Acids: Docosahexaenoic acid and eicosapentaenoic acid from omega-3 fatty acids in fish oils and fish oil supplements have anti-inflammatory properties. These benefits patients with a variety of arthritis like rheumatoid arthritis.
- Vitamin D: Vitamin D is a fat-soluble hormone that is produced in your skin when you are exposed to sunlight through the conversion of cholesterol. You can also obtain Vitamin D through foods and supplementation. Vitamin D deficiency has been linked to chronic pain. While more studies need to be done to correlate its effectiveness with osteoarthritis, vitamin D may have beneficial effects for patients suffering from chronic pain. You will need to have your levels checked to make sure you are not over or under supplementing.
- Glucosamine: Glucosamine is an amino acid that’s found in your cartilage. It has the potential to alleviate symptoms from osteoarthritis in the knee and may contribute to joint preservation.
- Chondroitin: Chondroitin is a compound found in cartilage and other connective tissues. A study found that when chondroitin was taken alone or in combination with glucosamine, it improved pain in patients with osteoarthritis. Chondroitin also is low risk making it a popular supplement.
- Methylsulfonylmethane (MSM): MSM is an organosulfur compound found in humans, animals, and green plants. It has analgesic and anti-inflammatory properties and by itself can relieve painful osteoarthritis. When taken in combination with glucosamine, this showed better efficacy in reducing pain, swelling, and improving joint function.
- Probiotics: Gut health plays a role in modulating our innate and acquired immune responses. Immune responses relate to our body’s inflammatory responses. Probiotics may contribute to reducing your body’s inflammation which is beneficial for osteoarthritis.
- Cannabinoids (CBD): CBD has gained popularity in our society. It has anti-inflammatory and analgesic properties that are beneficial to patients suffering from osteoarthritis.
- Bromelain: Bromelain is an extract from a pineapple plant and has demonstrated anti-inflammatory and analgesic properties in patients with osteoarthritis. It’s a great natural alternative to pharmaceutical drugs.
Be sure to consult with your doctor before starting supplements. This is extremely important especially if you’re currently taking medications and/or have other diagnosed medical conditions. If you prefer not to take a supplement, you can also increase your intake of natural foods that contain these ingredients.
- Exercise
Exercise not only helps your brain and heart, but it can help your joint health. However, it’s really important that you’re performing the correct form of exercise because certain movements can increase pain from osteoarthritis.
Remember: You want to make sure that the exercise you’re performing is not putting too much force and strain on your joints.
“Positive exercises” can prevent the development of osteoarthritis by strengthening your muscles. These exercises include:
- aquatic exercising like swimming
- aerobic exercise like walking, bicycling or jogging
- strengthening exercises like properly lifting weights, pilates, certain types of yoga
“Negative exercises” include exercises that cause pain to your joints. While lifting weights is excellent for gaining and retaining lean muscle mass, you want to make sure you are doing it properly so as to not put excess stress on the affected joints. This is where a physical therapist and/or a great personal trainer are key to your success. They’ll be able to customize a workout plan for your osteoarthritis. Exercise can also help you lose weight which will prevent excessive stress on your joints.
Living With Osteoarthritis
While there isn’t a specific cure for osteoarthritis, there are natural ways that you can manage the pain to improve your symptoms. Talk with your doctor if the pain is severe because medication or surgery may be needed.
Which of the three natural ways do you plan to incorporate? Let me know in the comments below.
And if you’re interested in learning more about natural therapies, call to book an appointment at 602-892-4727 or fill out our contact form.