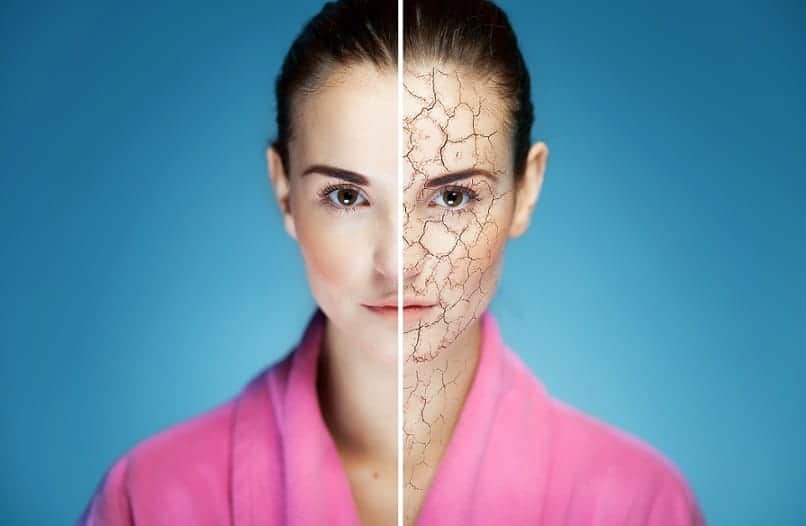
Rashes. Blisters. Tight skin. Scales.
Your skin looks great in old photos, but now you’re frustrated. Your skin quality is not what it used to be, and you want to cover up at all times – even on the hottest days of summer. You feel unattractive, and the usual soothing cream isn’t doing anything.
But did you know that many rashes are caused by autoimmune disease?
Yes, your immune system may be overreacting, causing those patches of skin you’d rather not look at. As these rashes can often be a warning sign of poor overall health, it may be time to get it checked out by a doctor.
What Is Psoriasis?
Psoriasis occurs when the lifecycle of your skin cells speeds up – and they multiply sometimes up to 10 times faster than normal. This causes a build-up of skin, often creating bumps and silvery scales – commonly found on your elbows, knees, scalp, and lower back.
Psoriasis Symptoms
Psoriasis symptoms manifest in a number of ways, including:
- Dry, cracked skin that can bleed
- Thick silvery scales covering red patches of skin
- Thickened, ridged, or pitted nails
- Flaking skin on the scalp
You may also experience associated symptoms such as an itching, burning, or a sore sensation in the affected areas. And sometimes you may have stiff or swollen joints alongside the skin issues – psoriatic arthritis.
What Is the Main Cause of Psoriasis?
Although the full mechanism behind psoriasis is still not completely understood, the main cause of the disease is inflammation and the immune system subsequently attacking healthy skin tissue – causing discomfort and itchiness and triggering your skin cells to multiply on overdrive.
Many patients with psoriasis also have other medical diagnoses, like high cholesterol, cardiovascular issues, higher BMI, or type 2 diabetes. It’s clear that psoriasis is a continuation of a metabolic and autoimmune status – and that there are greater implications than the condition of the skin.
Common psoriasis triggers include:
- Infection – can be in the skin, or elsewhere, for example: Strep throat
- Skin injury – bug bite, cut, severe sunburn
- Smoking
- Drinking a large amount of alcohol
- Stress of any kind
- Certain medications
- Nutrient deficiencies like Vitamin D, Vitamin A, or Omega-3 fatty acids
- Toxin exposure
Psoriasis can be managed, but it involves counteracting the underlying inflammation and immune system dysfunction, not just treating the symptoms topically.
What Is Lichen Sclerosus?
Lichen sclerosus is a chronic inflammatory skin disease that may be under-reported owing to the location of the rash. Lichen sclerosus affects the genital and anal areas, and it’s characterized by patchy, white skin that looks thinner than normal. These whitish patches and nodules can eventually merge to create larger sections called plaques.
Lichen sclerosus symptoms include:
- Severe itchiness (for women in the vulva area)
- Fragile, thin skin
- Soreness and pain
- Pain during sexual intercourse for women
- Erectile dysfunction in men
- Difficulty urinating
- Constipation
Like psoriasis, lichen sclerosus occurs when your immune system is on high alert, to the extent that many women with it also have a diagnosis of another autoimmune disease.
What Are the Risk Factors for Lichen Sclerosus?
Like any other autoimmune disease, lichen sclerosus has a number of risk factors that can contribute to the disease.
These include:
- Being a postmenopausal woman
- Having another autoimmune disease – such as a thyroid disorder, inflammatory bowel disease, alopecia, rheumatoid arthritis, psoriasis
- A relative with lichen sclerosus
- Previous trauma in the area
Lichen sclerosus is a chronic disease, so it’s important to not only ease your uncomfortable symptoms, but to look at ways of reducing the underlying inflammation – by managing any preexisting autoimmune disease and ensuring your hormone levels are optimized.
What Is Scleroderma?
Scleroderma (also known as systemic sclerosis) is a group of autoimmune rheumatic diseases that center on your skin, connective tissue, and blood vessels. Your skin may be the only area where you notice symptoms, but it can be a sign that connective tissue and blood vessels are also affected.
Collagen is a fibrous protein that makes up your connective tissue and skin. It’s responsible for giving your skin elasticity, volume, and strength, and for keeping structure inside your body. Scleroderma occurs when too much collagen is produced and kept in your body tissues. This is triggered by an overworked immune system – inflammation and immune cells attacking otherwise healthy connective tissue.
Symptoms of scleroderma include:
- Hardened, tightened patches of skin in straight lines or ovals. These can cover large areas of the body. Size, number, and location of these patches depends on the subtype of scleroderma. The patches may appear shiny, and it may be difficult to move the affected area as the skin is so tight.
- Raynaud’s disease – where your fingers or toes can turn blue and feel tingly or numb. It’s a sign that scleroderma is affecting your blood vessels.
- Digestive issues – depending on what part of your digestive system is affected, you may experience heartburn, bloating, difficulty swallowing, stomach cramps, constipation, or diarrhea.
If left untreated, scleroderma can cause severe complications and serious problems with your mouth, fingers, digestion, lungs, heart, and kidneys
A scleroderma diagnosis may require a physical exam, blood tests for specific antibodies, imaging tests to check your internal organs, or a skin biopsy.
What Is Alopecia?
Alopecia areata is a condition where small patches of hair fall out, which initially may not be obvious. When these patches connect up, it becomes more noticeable and can cause a loss of confidence in many patients. It’s patchier than the loss of hair in male pattern baldness and doesn’t thin out like with female pattern baldness. The condition can develop slowly or come on suddenly very fast. It can affect the scalp, eyebrows, eyelashes, and face. Alopecia universalis is where there is total hair loss.
The hair loss is unpredictable and regrowth is spontaneous. Because of this unpredictability it’s possible you may live with flare-ups of hair loss for the rest of your life – or it may only occur once.
Is Alopecia an Autoimmune Disease?
Alopecia areata is an autoimmune disease that occurs when your immune cells mistake healthy tissue for a threat from the outside. In the case of alopecia, your immune system specifically attacks your hair follicles, causing them to shrink. Hair follicles are both an anchor for your hair, and the sac that the hair strand grows out of, so if it’s damaged, it can no longer produce hair.
There may be a genetic component to developing alopecia, alongside environmental and hormonal factors – and experiencing stress and nutrient deficiencies. Stress can have a huge bearing on many autoimmune diseases. Alopecia is more likely to occur in patients with existing autoimmune diseases, such as rheumatoid arthritis.
Though alopecia can be distressing and can knock your confidence, there are ways to improve the outlook and target the underlying inflammation and autoimmunity without taking immunosuppressant drugs.
What Is Pemphigus?
Pemphigus is a group of autoimmune diseases where you experience painful blisters on your skin and mucous membranes. Your mucous membranes are found in your mouth, nose, throat, lungs, genitals, and eyes (your conjunctiva). The blisters are caused when your immune system targets the squamous cells that make up these moist parts of your body. When the tissues are damaged, it causes a breakdown in the connections between the cells.
Symptoms of pemphigus include:
- Painful blisters – these start off on your skin, or in your mouth.
- Difficulty eating or swallowing due to blisters.
- Blisters on the top of the skin that come and go.
- Blisters that ooze, crust, or peel.
Certain types of pemphigus can be life-threatening in many cases, so it’s important to seek diagnosis and treatment – it’s far more than just a cosmetic issue.
How Is Pemphigus Diagnosed?
Your doctor or dermatologist needs to rule out other diseases while checking for pemphigus biomarkers.
Your doctor needs to organize the following tests:
- Physical exam – to check the condition of your skin, and the affected areas.
- Skin biopsy – examining the blistering underneath a microscope is one of the best ways to formally diagnose pemphigus.
- Blood test – to look for antibodies associated with pemphigus.
- Endoscopy – your doctor may need to check for sores in your throat and esophagus.
Once you have a diagnosis, treatment can begin, and you can focus on managing the disease long-term. You can aid your healing by adopting dietary and lifestyle interventions that can reduce the underlying inflammation.
Treating the underlying inflammation is crucial for managing any of these skin autoimmune diseases. After all, what gives lasting results – treating the symptoms, or understanding and counteracting the root cause?
If you want to get back to your old life, and spend less time thinking about applying topical creams, or dealing with nasty side effects from medications, it may be time to turn to functional medicine. Individualized treatment focused on giving you actionable advice, following extensive testing. You become empowered to make positive changes in your health.
We can help you in tackling the underlying causes of skin autoimmune disease or other autoimmune disease. If you’re interested in checking out functional medicine in the Phoenix, Scottsdale, Paradise Valley, Arizona area, call to book an appointment at 602 892-4727 or fill out our contact form. If you’re not local to us, why not try 7 Weeks to Your Healthiest Self – our masterclass that provides you with the lifestyle change benefits of functional medicine – from the comfort and privacy of your own home.